Pediatric Topics is a collection of information sheets given at each well child visit to assist you in learning more about your child. These information sheets can be saved in the green vinyl Pediatric Healthcare binder given at your child’s one month visit. The following links are a sampling of the subjects covered in the Pediatric Topics.
Please Note: All content on this website is intended for educational purposes only and should not be used as medical advice for the treatment of an illness or medical problem. In no way is this information intended to be a substitute for individual professional medical care. If your child has a medical need, please contact our office for an appointment.
Antibiotics & Infections
Antibiotics are medications that are prescribed to help the body fight bacterial infections. The primary classes of antibiotics used in children include the penicillins, the sulfas, the cephalosporins and the erythromycins. These medications are only effective in the treatment of bacterial infections and do not have any effect on common viral infections. The presence of fever with an illness does not always mean that a bacterial infection exists, nor does it mean that an antibiotic is necessary for treatment. In fact, most fever in children is caused by viral infections. Antibiotics are expensive, may cause allergic reactions, intestinal upset and other adverse effects and should be used only after a thorough examination has revealed a bacterial infection.
All children experience several infectious illnesses in their early years. A number of factors affect the frequency of these illnesses, but probably the most significant factor is the child’s exposure to other sick children. Attendance at daycare or schools generally leads to more infections. While some illnesses with fever may be harmless and self-limiting, others will require antibiotics to clear the infection. The decision to use antibiotics will be determined by a review of your child’s symptoms and a physical examination. Laboratory test or x-rays may also be needed. Once a bacterial infection is detected, antibiotics will be prescribed. Examples of illnesses requiring antibiotics include ear infection, sinus infection, pneumonia, urinary infection, impetigo, strep throat and joint infection.
When an antibiotic is prescribed, it is important to fully complete the recommended course of treatment. In general, this will be a minimum of 5-10 days. Though the child’s symptoms may improve in 3-4 days, the antibiotic should be taken until it is all gone.
In review, most childhood illnesses with fever are caused by viruses and do not require antibiotic therapy. If, however, a bacterial infection is discovered after a proper evaluation, an antibiotic will be prescribed. The body’s own defenses will adequately combat most viral infections and therefore antibiotics will afford no help in this case.
Bites, Stings, Cuts, & Burns
Accidents in childhood, including bites, stings, and cuts, constitute some of the more frequent medical problems beyond the age of infancy. Proper care and precautions will prevent a number of accidents and reduce the severity of others. Despite the best of care, however, some accidents occur. The following first aid measures are generally helpful when they do.
Animal Bites
Children should be taught to be wary of unfamiliar dogs or cats, and should not be left alone with any pet. If a child is bitten, scrub the bite area well with soap and water for a few minutes, and apply an antibiotic ointment. Notify the animal control authority, sheriff or police. Dogs and cats should be confined for 10 days of observation even if the rabies shots are up to date. Call the office for severe bites, deep cuts, or signs of infection.
Signs of wound infection include yellow fluid drainage, redness of surrounding skin, red streaks radiating from the wound, increasing pain, or significant fever.
Insect Stings & Ant Bites
The risk of bee stings can be reduced by avoiding areas where bees feed or congregate (fields with flowers, blooming trees, and bird baths). Children should be taught to recognize and avoid ant beds. If a child is stung, remove the stinger, if present, using a scraping motion with a plastic card or fingernail. Apply ice or cold compresses periodically for 8-10 hours to minimize the swelling. Benadryl will help relieve itching and swelling. The application of a teaspoon of moistened papain (Adolf’s Meat Tenderizer) for 15 minutes may neutralize some of the toxin, but will not aid ant bites. Most children will develop a local reaction of swelling, redness, and warmth. Stings on the hand or foot can cause swelling of the entire hand or foot. A sting near the eye may cause the eyelid to swell shut. Contact a physician if the child develops generalized rash, wheezing, hoarseness, facial or tongue swelling, faintness or for any signs of infection.
Signs of wound infection include yellow fluid drainage, redness of surrounding skin, red streaks radiating from the wound, increasing pain, or significant fever.
Cuts & Scrapes
Bleeding from an injury can usually be stopped within 10 minutes if direct pressure is applied to the wound. Cleanse the wound well with soap and water, apply an antibiotic ointment, and cover with a sterile dressing. If the cut is deep or the edges gape open, suturing may be needed for proper healing. Call the office if signs of infection occur. A tetanus booster is given within 72 hours for significant cuts, contaminated abrasions, puncture wounds, bites and burns. A booster dose is needed if a child had not completed a primary immunization series (2,4,6, and 18 month shots) or received a booster dose within the preceding five years. Call our office for any tetanus immunization questions.
Signs of wound infection include yellow fluid drainage, redness of surrounding skin, red streaks radiating from the wound, increasing pain, or significant fever.
Burns
Burns in childhood most commonly occur from touching curling irons, hot water, hot drinks, hot grease, and hot mufflers. The burn is usually first degree (reddened skin without blisters) or second degree (with blisters). Neither of these will typically leave a scar. Second-degree burns take up to 3 weeks to heal. A third-degree burn is deep, may leave areas of charred skin, and often requires a skin graft to properly heal. Immediately put the burned part of the body in cold water, or pour cold tap water over it for 10 minutes. If you are outside, the nearest garden hose should be used. This will lessen the depth of the burn and relieve pain. If the burned area is large, cover it loosely with a clean sheet or plastic wrap. The covering will keep the burn clean and reduce the pain. All second and third degree burns will require evaluation by a physician.
Daily Care of Burn Wounds:
- For pain, put cold wet cloths on the burned area and take acetaminophen every 4 hours or ibuprofen every 6 hours for at least 24 hours.
- Wash the area gently with liquid soap twice a day. If blisters are present, don’t open them – the outer skin protects the burn from infection. When the blisters break, gently clean the site daily, apply an antibiotic ointment (such as Bacitracin or Polysporin) and cover the burn site with a Band-Aid or sterile gauze dressing.
- After the blisters have broken, the dead skin needs to be timed away with fine scissors. This prevents infection from forming within the hidden pockets of the dead skin. The physician may ask to see the child every 2 or 3 days to perform this task of debridement.
- A blister is larger than 2 inches across
- The burn is on the face, hands, feet, or genitals
- It was an electrical burn
- It starts to look infected
- You have any questions or concerns
- Acetaminophen (Tempra, Tylenol) may be offered for fever and body aches. Avoid the use of aspirin and other salicylates with chicken pox due to the possibility of Reye’s Syndrome.
- Oral anti-itch medication, such as diphenhydramine (Benadryl), maybe offered as needed.
- The child should avoid excessive scratching of the rash as this may lead to bacterial infection of the sores.
- Lotions, such as Calamine, may be applied to relieve itching. Baking soda or oatmeal baths (Aveeno) may also be soothing to the rash. A child may hold an ice cube against a particularly itchy spot for a few minutes for temporary relief.
- An area of the skin becomes red, swollen, and painful. This could indicate the presence of a bacterial skin infection for which the doctor can prescribe oral antibiotics after evaluation.
- The child develops difficulty breathing or chest pain. These are symptoms of pneumonia which rarely accompanies chicken pox in children but frequently affects adults with the disease.
- The child begins to vomit or become disoriented during or after the illness. These are symptoms of Reye’s Syndrome, a serious disease that follows viral infections such as chicken pox. Reye’s Syndrome has been liked to aspirin use during viral illness. Therefore, never give aspirin to children with chicken pox, influenza, or other viral infections.
- Clear the nose of mucous with a rubber bulb syringe before each feeding and before naps, if feeding or sleeping is impaired.
- Use saline nose drops to loosen mucous if necessary. This may be purchased at a drug store or mixed at home using ¼-teaspoon salt in one 8-ounce cup of lukewarm water. Place one to two drops of saline solution into one nostril, suction with the bulb syringe and repeat for other nostril.
- Run a cool-mist humidifier in the infant’s room if the interior air is dry. Do not run the humidifier continuously for weeks or months as this can promote allergies to mold.
- Offer plenty of liquids. A baby with a cold will often refuse formula and solids, but will take Pedialyte, Infalyte, Gatorade, or juices.
- Give acetaminophen (Tempra, Tylenol) for fever or discomfort as needed.
- Encourage the child to rest with quiet activities.
- Run a cool-mist humidifier at night if the interior air is dry. Do not run the humidifier continuously for weeks as this can promote allergies to mold.
- Offer plenty of liquids to drink. The child with a cold will often refuse most solid foods and milk, but will take Gatorade, fruit juice, Popsicles and fruit snacks.
- Give acetaminophen (Tempra, Tylenol) for fever or discomfort.
- Give symptomatic cold medication such as Dimetapp, Sudafed, Triaminic, or Pediacare (all are over-the-counter). See the Medication Dosing Chart for dosage.
- Offer plenty of fluids to drink.
- Run a cool-mist humidifier at night if the interior is dry. Avoid continuous use of the humidifier vaporizer as this may cause a build-up of molds in the room.
- Keep the bedroom cool during sleep.
- Use a cough medicine with dextromenthorphan (DM) at nap and bedtime, such as Pediacare Night Rest or Triaminic Nighttime.
- Wrap the child warmly and take him outside into the cool air. The humid, cool air will help the breathing and the distraction of outdoors will help calm the child.
- If the breathing difficulty persists, run hot water through the showerhead for five minutes to steam up the bathroom. Then take the child into the steamy air for five minutes.
- Repeat step one, if needed.
- If significant breathing difficulty persists, contact a physician.
- Lightly clothe the child to allow the body to lose its excess heat.
- Encourage the drinking of cool liquids and eating of Popsicles as tolerated.
- If the child is uncomfortable, give a fever medication: acetaminophen (Tempra, Tylenol) or ibuprofen (Advil, Motrin). If the fever is greater than 101°, use acetaminophen, and if greater that 102.5° use ibuprofen. For fever persistently above 103°, doses of acetaminophen and ibuprofen may be given together. Antibiotics and over-the-counter medications may be given along with fever medications.
- Sponge baths to reduce fever are usually not necessary. Exceptions would be emergencies such as heat stroke, delirium from fever, a seizure from fever or fever over 106°. Do not sponge with alcohol or ice water. Place the child in about two inches of lukewarm bath water and sponge the water slowly over the head, shoulders, chest, and back. The child’s body temperature will slowly fall, but don’t expect the fever to drop below 101°.
- Fever lasting longer than three days. Fever caused by most viral infections usually resolves within three days.
- Fever associated with a stiff neck, severe headaches, or excessive drowsiness.
- Fever with pain in a specific part of the body such as an earache, sore throat, neck pain, or painful urination.
- Fever with the sudden appearance of a skin rash.
- Is the skin broken? Most bleeding is controllable with direct pressure over the wound for 10 minutes. Wash small cuts or abrasions with soap and water. Deep or gaping cuts may need suturing for proper healing. (See Topic 15 sheet).
- How did the injury happen? The greater the force behind the injury, the greater the concern. An automobile accident, a long fall (as from a roof), and an impact from a heavy object (as from a baseball bat) are examples of significant force.
- Was there any loss of consciousness? Either being “knocked out” or having a seizure is indicative of loss of consciousness. Any loss of consciousness, however brief, may signal a dangerous head injury and requires immediate medical evaluation of the child.
- Does the child have a headache of increasing intensity? Headaches are common after a head injury, but generally improve fairly rapidly. A headache that is becoming more severe requires immediate medical attention.
- Has the child vomited? One or two episodes of vomiting are common immediately following a head injury. Any vomiting more than two hours after the accident is reason for concern, especially if it is associated with a headache.
- How is the child acting? Confusion, disorientation, excessive sleepiness, blurred or doubled vision, unsteady walk, weakness in arms or legs, and difficulty speaking are indications deserving immediate medical attention.
- If sleepy immediately after the head injury, allow the child to rest or sleep. Sleepiness is common due to exhaustion from the pain and agitation of the accident. Wake the child in one hour to access his alertness.
- Give only clear fluids (no solid foods) until the child has gone six hours without vomiting.
- Don’t give the child any medication that may cause drowsiness, such as antihistamines. Acetaminophen (Tempra, Tylenol) or ibuprofen (Advil, Motrin) are acceptable for pain relief.
- Observe the child closely for 48 hours. Awaken him three times during the night: once at your bedtime, at 1:00 a.m. and at 4:00 a.m. More frequent checks may be necessary if advised. Arouse him until he is walking and talking normally.
- Call back if:
- The headache worsens.
- The child has any vomiting two hours after the accident.
- The child is difficult to arouse, acts confused or is unable to walk.
- If there are any unusual symptoms, such as neck stiffness, vision problems, speech difficulty or fluid drainage from the ear or nose.
CALL THE OFFICE IF:
Signs of wound infection include yellow fluid drainage, redness of surrounding skin, red streaks radiating from the wound, increasing pain, or significant fever.
Chicken Pox
Previously, about 3 1/2 million people would contract chicken pox each year, but with the introduction of a vaccine this infection is much less common today. The highly contagious illness is most common among children between ages one and nine. Adolescents and adults are usually immune because of childhood infection, but usually have more difficulty with chicken pox if they contract it.
A widespread rash, beginning on the truck and spreading to the arms, face and scalp, is the most prominent symptom. The rash begins as a crop of small red spots, which quickly become raised, fluid filled blisters. These blisters then break and form yellowish scabs. As the initial rash crusts over, new spots appear. At the height of the illness, spots, blisters, and scabs are all present on the skin. Once all the blisters have crusted over, usually seven days after the first breakout, the disease is no longer contagious.
Chicken pox travels from child to child via airborne viral particles shed from the respiratory passages and blisters. After it enters a child’s system, the virus incubates for 14 to 21 days before the rash appears. For 24 hours before the rash appears the disease is contagious, so it is not always possible to avoid exposure.
Treatment
There is no curative treatment for chicken pox infection. Many children have symptoms so mild that no medication is needed. Most, however, will have low-grade fever, fatigue, itching and generalized discomfort.
Possible Complications
Chicken pox is generally a mild illness. There is usually no need to keep the child with chicken pox in bed. The purpose of staying home is mainly to avoid infection other children. Some children, however, run fevers as high as 104. Painful sores inside the mouth or in the rectum or genitals are also not uncommon.
More serious complications, while rare, do sometimes occur. Call your doctor immediately if:
Chicken Pox Vaccine
The chicken pox vaccine (Varivax) is recommended for children over 12 months of age. It is 85% effective in preventing the infection and it reduces the severity of the disease in those immunized individuals who get chicken pox. Life long immunity is promising, but uncertain at this time.
Cold
The common cold is caused by several different viruses and has thus far escaped cure or prevention. The symptoms of a cold include watery eyes, runny nose, scratchy throat and sneezing. A child may also have low-grade fever congestion and a cough. Most colds are self-limited and will run their course in 5-20 days. In general, children three months to three years old have more frequent colds (average 5-8 each year) and symptoms that last longer. Children in group settings, such as school and day care, also have more viral infections due to their greater exposure to other children.
A child with a cold is most contagious to others in the first 72 hours of the illness. If fever is present, the child should not attend school or day care. These viral infections are usually spread by coughing, sneezing, hand-to-hand contact, and contact with contaminated objects.
Despite symptomatic treatment, colds will last an expected 5-10 days. Since they are viral infections, antibiotics are not used unless complications arise. Medicated nose drops or sprays, such as Neosynephrine or Afrin, may cause persistent nasal congestion and should not be use unless specifically recommended.
A discolored nasal discharge is not necessarily an indication for antibiotics. The nasal discharge of the common cold will typically change from a clear discharge, to cloudy, to discolored (yellow or green), then resolve without treatment. If the nasal discharge has lasted more than 10 days, is discolored and is not improving, then sinusitis may exist and a doctor should be consulted.
Colds may lead to complications or have other illnesses mistaken for them. Indications for medical attention include high fever or fever occurring several days after the onset of illness, significant sore throat, severe headache or facial pain, difficulty breathing not solved by clearing the nose, excessive sleepiness or irritability, or a child who appears more than mildly ill.
The following give guidelines for the symptomatic treatment of a cold.
Infants
Older Children
Cough
Cough is a protective mechanism used by the body to rid the airway and lungs of foreign matter. Most coughs accompany viral upper respiratory infections (colds) and are the result of airway irritation or mucous draining down the upper airway. Cough may also be a symptom of pneumonia or an asthma attack. If the cough is associated with rapid or labored breathing, a physician should be consulted at once. Otherwise the cough associated with a cold can be temporarily managed as follows:
Croup
Croup is an acute viral respiratory infection involving the upper airway passages. It results in swelling of the vocal cords and narrowing of the upper airway to produce the symptoms of croup: hoarse voice, barky cough, labored breathing and low-grade fever. Croup may be preceded by a mild cold, or may occur unexpectedly. Typically, the symptoms of croup have an abrupt onset between 10 p.m. and 2 a.m. Croup generally improves during the day and worsens each night for 3-4 days.
With the acute onset of croup in the evening, the child’s breathing difficulty will generally improve 15-20 minutes. In order to hasten improvement, try the following:
When the breathing has improved, the child may be returned to his bed and a cool-mist humidifier set up to blow directly over the bed. A cough suppressant may be given as well.
Severe breathing difficulty not responding to steam or cool air, high fever, excessive drooling or undue apprehension are danger signs which call for immediate physician notification. In addition to these, a child who has had more than mild breathing difficulty should be examined in the office the following day.
Ear Infections
Earache is a common occurrence in childhood and may have a number of causes. Infected fluid may accumulate behind the eardrum, or external ear canal may become infected. Children may also complain of ear pain with a sore throat.
Middle Ear Infection
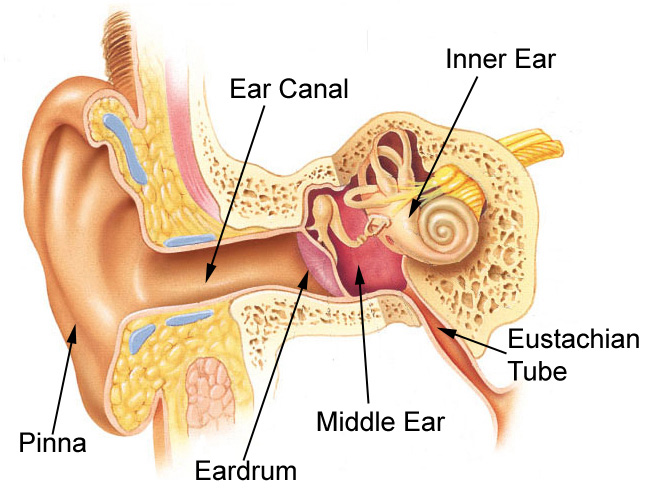
Middle ear infection is a common complication of a cold in children. The middle ear space lies behind the eardrum and contains three tiny bones that transmit sound to the nerve endings of the inner ear. The Eustachian tube ventilates the middle ear space into the back of the throat. Swelling and congestion due to a cold may obstruct the Eustachian tube and allow fluid to fill the middle ear space. This fluid may then become infected.
Indications of middle ear infection include irritability, sleeplessness, earache and fever. Infants may or may not tug or rub the ear. Infants may also have vomiting or diarrhea associated with an ear infection.
The pain of a middle ear infection can often be relieved with acetaminophen (Tylenol) and heat applied to the external ear with a heating pad or warm compress. If there is no ear canal discharge, numbing drops, such as Auralgan or Otocaine, may be used. Ear pain will usually subside after a few hours but the infection will remain. The child should be checked within a day after onset of symptoms. Note: Numbing drops should not be given to a child who has tubes in the eardrum.
Middle ear infections are generally treated with an oral antibiotic. If a child has not shown improvement within 2-3 days, the ears should be checked again. Regardless, the child should be checked a few days after completing the antibiotic to be sure the infection and fluid have resolved.
External Ear Infection
External ear infection (swimmer’s ear) is an infection of the ear canal down to the eardrum, which may affect the middle ear space as well. Moisture trapped within the ear canal damages the skin and encourages the growth of bacteria or fungi. The main symptom is ear pain, which often begins gradually and increases with continued exposure to water. Mild soreness of the ear may be treated with drying alcohol-based ear drops (Swim Ear). If the pain is persistent or an unusual discharge is noted from the ear, the child should be examined.
Other Causes:
Ear pain may also be caused by middle ear pressure with or without fluid, dental problems, local skin conditions and foreign bodies in the ear canal. In general, ear pain that is severe, persistent, or associated with a cold, fever, or other signs of illness may be serious and does require a physician’s examination.
Fever
Fever is the body’s natural response to infection and may be quite helpful in fighting the infection. Fever is defined as a rectal temperature over 100.5°F, an oral temperature over 100°F, or an axillary (under arm) temperature over 100°F. The body’s average temperature of 98.6° may normally fluctuate from 97° in the morning to a high of 100° F in the evening. Exercise, excessive clothing, hot weather, and warm drink may cause mild elevations of temperature. For this reason, low-grade temperatures should be retaken one hour later to verify their existence.
For children under three years, the most accurate method of temperature measurement is rectally. Axillary measurements can give general estimates of body temperature. Oral measurements are practical beginning at three years of age. Ear thermometers are useful with older children, but are inaccurate with children under 6 months and difficult to properly use under 2 years of age.
Most childhood fevers are caused by viral infections that require no treatment and last from one to three days. Other causes of fever include infections of the ears, sinuses, throat, urinary tract, lungs and skin. In general, the height of the fever and the effectiveness of fever medication in lowering the temperature are not related to the seriousness of the infection. What is more important is the child’s appearance and general disposition during the illness. Many children with viral infections tolerate temperatures as high as 103° F without any significant change in activity – this is a favorable sign that the condition is not serious. Other children with temperature elevations may be particularly irritable, excessively sleepy, or may complain of pain in a certain part of their body. These children will require a medical evaluation to determine the cause of their fever.
Since fever is not harmful to the body, it need only to be treated if a child is experiencing some discomfort as a result. Low-grade fever is usually well tolerated, but fever of 102°F or higher may cause a child to feel poorly. The following measures will help reduce the fever.
Although fever aids the body’s defenses in fighting infection and is not harmful to the body, an occasional child may have a seizure with high fever. These seizures are generally of short duration (less than five minutes) and result in no brain damage. They are generally caused by a rapid rise in body temperature, and therefore are not easily prevented. If your child does experience a seizure, lay him on the floor on his side away from any objects that he might strike with his arms or legs during the seizure. Don’t try to force anything into your child’s mouth since tongue swallowing is not possible. An immediate examination by a physician is recommended.
Each of the following conditions will require consultation with a pediatrician or the office staff:
Fever above 101° rectally in a child less than four months of age.
Head Injuries
Head injuries are common in childhood, especially during the early developmental years. Most are not serious and result in no noticeable injury to the head. More forceful blows to the head may result in an abrasion, a deep cut or a lump on the scalp due to broken blood vessels under the skin. Most attention, however, must be focused upon the child’s mental and neurological state. The following guidelines will help in assessment and treatment of a head injury.
Home Management of a Mild Head Injury
Once the child has been evaluated, or determined to have sustained only a mild head injury, the following steps should be followed:
Medications for the Home
The following medications can be purchased without a prescription and are recommended for the condition under which they are listed. Many of these over-the-counter medications are equally as effective as prescription medications. If these medications are ineffective in controlling the condition, the doctor may prescribe an alternative.
Cuts & Abrasions:
Use an antibiotic ointment on small cuts and abrasions after a thorough cleaning with soap and water. Examples: Neosporin, Polysporin and Bacitracin.
Diaper Rash:
A cream may be applied after every diaper change. Examples: Resinol, Balmex, Desitin, and Zinc Oxide. If a yeast infection is suspected, also apply a medicated cream three times a day, such as Lotrimin AF.
Allergic Reactions & Insect Bites:
Diphenhydramine (Benadryl or generic) elixir may be given by mouth to reduce the symptoms. The dosage is listed in the table below under Allergic Symptoms.
Sore Throat:
Lozenges and Chloraseptic Spray may help relieve the pain.
Poisoning:
See the “Poison Prevention” page.. Call the Poison Control Center in Birmingham at 1-800-292-6678, or our office for advice.
Fever:
Acetaminophen (Tylenol) or Ibuprofen (Advil, Motrin).
Itching Rash:
Calamine Lotion and colloidal oatmeal (Aveeno) or baking soda baths may be helpful.
Sore Throat
Sore throat is one of the most common medical complaints of children. There are many causes of sore throats, including viral infection, bacterial infection, mouth breathing, and allergic states.
Colds, laryngitis, and croup are viral infections that are associated with a sore throat. Mononucleosis is a viral infection which causes fever, sore throat, and swollen glands. It is more common in adolescents. Viral infections do not require antibiotic treatment and are properly controlled by the body’s own defense mechanisms. The resulting sore throat is best managed by drinking cool liquids, getting plenty of rest and by taking acetaminophen (Tempra) for pain-relief.
A bacterial infection of the throat is almost always caused by the Streptococcus bacteria. Strep throat is most common in the school-aged child and is seen less frequently in children under two years old. Symptoms may include sore throat, swollen glands, fever, headache, nausea, and abdominal pain. A red rough rash over the body may be associated with it as well. Accurate diagnosis by a Streptococcal antigen test or a throat culture is necessary for proper treatment to be prescribed. Untreated Strep throat may occasionally result in serious complications such as acute rheumatic fever.
Irritative or allergic nasal problems with associated postnasal drip may cause a sore throat. These symptoms can often be relieved by an antihistamine or decongestant (see Medications for the Home), or by avoidance of the offending allergic agent if it can be identified.
In general, a child with a mild sore throat, without fever and who otherwise feels well may be safely observed at home for a day or two and offered acetaminophen (Tylenol, Tempra) for pain relief. A child who is acting ill and has symptoms of Strep throat, as stated above, will require a medical evaluation.
Television Precautions
Television has a tremendous influence on how children view our world. Most youngsters spend more hours watching TV from birth to age 18 than they spend in the classroom. A positive aspect of TV viewing can be the opportunity to see different life-styles and cultures. In addition, TV has great entertainment value. While TV can be a good source of instruction, most children watch TV excessively and experience some of the negative consequences described below. Many of these same concerns apply to video games, computer games and exposure to the Internet.
Harmful Aspects of Television
TV displaces active types of recreation.
It decreases time spent playing with peers. A child has less time for self-directed daydreaming and creative thinking. It takes away time for participating in sports, music, art, or other activities that require practice to achieve competence.
TV interferes with conversation and discussion time.
It reduces social interactions with family and friends.
TV discourages reading.
Reading requires much more thinking than watching television. Reading improves a youngster’s vocabulary. A decrease in reading scores may be related to too much time in front of the TV.
Heavy TV viewing (more than 4 hours a day) definitely reduces school performance.
This much TV interferes with study, reading, and thinking time. If children do not get enough sleep because they are watching TV, they will not be alert enough to learn well on the following day.
TV discourages exercise.
TV watching promotes an inactive life-style, which leads to poor physical fitness. If accompanied by frequent snacking, watching TV may contribute to weight problems.
TV advertising encourages a demand for material possessions.
Young children will pressure their parents to buy the toys they see advertised. TV portrays materialism as the “American way.”
TV violence can affect how a child feels toward life and other people.
Viewing excessive violence may cause a child to be overly fearful about personal safety and the future. TV violence may numb the sympathy a child normally feels toward victims of human suffering. Young children may be more aggressive in their play after seeing violent television shows.
Preventing Television / Media Addiction
Avoid TV viewing for children under the age of two years.
Research on early brain development shows that babies and toddlers have a critical need for direct interactions with parents and caregivers for healthy brain growth and the development of appropriate social, emotional, and cognitive skills. Therefore, the American Academy of Pediatrics recommends that young children be discouraged from watching TV programs.
Encourage active recreation.
Help your child become interested in sports, games, hobbies, and music. Occasionally turn off the television and take a walk or play a game with your child.Read to your children.
Begin reading to your child by 1 year of age and encourage him to read on his own as he becomes older. Some parents help children earn TV or video game time by equivalent reading time. Help him improve his conversational skills by spending more of your time talking with him.
Limit TV time to 1-2 hours a day for older children.
Limit TV to 1 hour on school nights and 2 hours a day on weekends. Occasionally you may want to allow extra viewing time for special educational programs.
Be selective of the TV programs your children watch.
Choose programs for their moral and instructive value, not just for entertainment. Avoid programs that display disrespectful social relations or disharmonious parent-child relations. Co-view with your child and discuss the content of the programming.
Don’t use TV as a distraction or a baby-sitter for preschool children.
Preschooler’s viewing should be limited to special TV shows and occasional videotapes that are produced for young children. Because the difference between fantasy and reality is not clear for this age group, regular TV shows may cause fears.
If your child is doing poorly in school, limit TV time to 1 half hour each day.
Make a rule that your child must finish homework and chores before watching television. If your child’s favorite show is on before the work can be done, consider recording the show for later viewing.
Set a bedtime for your child that is not altered by TV shows that interest your child.
Children who are allowed to stay up late to watch television are usually too tired the following day to remember what they were taught in school. By all means, do not permit your child to have a TV set in her bedroom because this eliminates your control over TV viewing and is associated with sleep problems, school dysfunction, and childhood.
Turn off the TV set during meals.
Family time is too precious to be squandered on TV shows. In addition, don’t have the television always on as a background sound in your house. If you don’t like a quiet house, try to listen to music without lyrics.
In summary, limited TV viewing for the older child can be an entertaining and educational experience. As with most matters, however, too much of a “good thing” can be detrimental.
Viral Infections
Many childhood illnesses are the result of viral infections. Viruses cause over 70% of childhood respiratory illnesses and 80% of intestinal infections. The virus is a microscopic organism passed from person to person by coughing, sneezing, and hand-to-hand contact. Unlike bacteria, viruses are unaffected by antibiotics, but are generally well controlled by the body’s own immune defenses.
Viruses often distinguish themselves by the signs and symptoms they cause. The chicken pox, measles and rubella viruses are known for the characteristic rash and discomfort they cause. Mumps virus produces swelling of the salivary glands, and influenza virus causes a long-lasting illness with fever, muscles aches and cough. The poliovirus is known for the nerve damage it causes. The mononucleosis virus causes sore throat, fever, and prolonged fatigue. Other viruses, however, produce only general symptoms such as fever, runny nose, cough, vomiting, or diarrhea. These viruses do not have commonly recognized names.
Currently, the only effective treatment for most viral infections is the body’s own immune system which is possibly enhanced by fever. Children with viral infections causing symptoms such as runny nose, fever, headache, sore throat, muscle aches and fatigue will feel better with plenty of rest, good fluid intake, and pain medication (Tempra, Tylenol). Antihistamines and decongestants may be offered for congestion and anti-nausea medications may be useful for vomiting.
Occasionally simple viral infections will result in secondary complications requiring further evaluation. An ear or sinus infection may follow a persistent runny nose and congestion. Dehydration may result from persistent vomiting and diarrhea due to a stomach virus. A prolonged viral chest cold may lead to bacterial pneumonia. Given a few days, most children recover from viral infections without incident. If, however, new problems arise or the primary problem persists longer than expected, the child with a diagnosed viral illness should be re-evaluated by the physician.
Vomiting & Diarrhea
Vomiting and diarrhea are common symptoms associated with many childhood diseases. Though unpleasant for the child, these symptoms are not typically serious, are short lived and are generally controllable by diet. Vomiting will almost always cease if food and drink are withheld for 2-3 hours. Diarrhea will decrease if milk products and solid foods are withheld from the child’s diet for a day or two. Either vomiting or diarrhea by itself rarely leads to dehydration of a child.
When a child vomits, many parents immediately give medicine or sips of fluids to “prevent dehydration”. This usually causes more vomiting and worsens the child’s condition. Please closely follow our suggestions listed on the following:
Vomiting
Give nothing by mouth, including water, until there has been no vomiting for 1 hour (infants) or 2 hours (older children). Then begin offering fluids in frequent, small amounts.
First 8-12 Hours
Under 1 year: Oral electrolyte solution (Pedialyte, etc.)*
½ oz. every ½ hour for 3 times then,
1oz. every ½ hour for 3 times, then increase the amount as tolerated.
Over 1 year: Gatorade, half-strength Sprite or 7-Up, Popsicles
1oz. every ½ hour for 3 times then,
2oz. every ½ hour for 3 times, then increase the amount as tolerated.
Breast-feeding: Nurse every ½ hour for 5 minutes, alternating breasts. Increase
feeding time as tolerated. May supplement with an oral electrolyte solution
(Pedialyte, etc.)*.
If vomiting recurs, return to previous step in fluid introduction.
Next 12-18 Hours
After 12 hours with no vomiting, formula and solids may be added to the liquid diet. Offer small infrequent feedings at first.
Under 1 year: Formula, rice cereal, bananas, crackers, applesauce.
Over 1 year: Bananas, crackers, applesauce, toast, Jell-o, potatoes, soup.
Breast-feeding: Breast milk plus the above solid foods.
After 48 hours
After 48 hours with no vomiting, your child may return to a regular “light” diet, avoiding spicy and high fat foods. If vomiting recurs, then temporarily return to a liquid diet. If necessary, a child may go several days without eating solid foods without harm. The child’s intake of fluids is more important than the intake of solid foods. If vomiting persists, contact our office for advice.
*To improve the taste, ¼ teaspoon of pre-sweetened, sugar-free Kool-Aid powder may be added to 8 ounces of an oral electrolyte solution.
Diarrhea
With infection, diarrhea often follows vomiting. If the child is having fewer than four bowel movements per day, a regular diet should be continued, with gradual improvement expected. With four or more loose bowel movements per day, dietary changes may be helpful.
First 12 Hours – No solid foods in diet
Under 1 year: Offer electrolyte solution* such as Pedialyte.
Over 1 year: Clear liquids, such as Gatorade, 7-Up, Sprite, Cola, Popsicles.
Breast-feeding: Continue breast milk without solid foods.
After 12 Hours – Begin solid foods and formula
Under 1 year: Soy formula with cereal, bananas, crackers, and applesauce.
Over 1 year: Bananas, crackers, applesauce, toast, Jell-o, potatoes, soup.
Breast Feeding: Continue breast milk, plus cereal, bananas, applesauce, crackers.
After 48 hours
The child should return to a regular diet, even if the bowel movements are loose and frequent. Formula fed infants should continue the soy formula until the bowel movements have returned to normal, typically within 5 days. Fruit juices should be avoided until bowel movements have returned to normal.
The stool may be somewhat loose 3-5 days, but their frequency should decrease to 2-3 stools per day. If profuse diarrhea persists or blood is noted in the stools; contact our office for advice.
The major complication of vomiting and diarrhea is the loss of body fluids resulting in dehydration. Signs of this condition include infrequent urination (less than three voids in 24 hours), dry mouth, lack of tears when crying, or excessive drowsiness. Contact our office if your child is displaying any of these signs.
*To improve the taste, ¼ teaspoon of pre-sweetened, sugar-free Kool-Aid powder may be added to 8 ounces of an oral electrolyte solution.